Biophotonics
The field of biophotonics sits at the interface of optics and biology. We use light both to study the properties of biological systems and also to develop new tools for medical and environmental applications.
In a collaboration with marine biologists at the Lyell Centre, we are studying the process of photosynthesis in deep-sea red coralline algae to understand how these systems can survive at depths to which very little sunlight can penetrate. We are also developing smart lighting systems for artifical growth of microalgae in photobioreactors, as a green pathway to biosynthesis of chemical feedstocks, and the sequestration of CO2.
Medical applications of organic semiconductors
The use of light for medical applications is growing. Organic optoelectronic devices can be used for sensing muscle movement and can be applied in prosthetics, where a flexible, comfortable organic optoelectronic device can be worn on the residual limb to measure signals from muscles and help control artificial limbs.
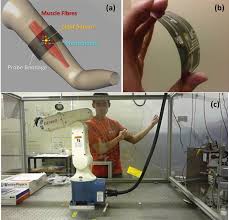
In the design of an active prosthetic device, the detection of a signal suitable as a trigger or as a proportional controller for the prosthesis actuation is among the key issues. Using an optical technique is appealing, as they are intrinsically free from electromagnetic noise and are not invasive on the tissues. The near-infrared optical absorption of muscle is dominated by blood and as such, during contraction, the muscle undergoes blood depletion. It has been demonstrated that the contraction can be detected as a decrease in the optical absorption of the muscle.
Light can also be applied in the treatment of many diseases. Photodynamic therapy (PDT) uses light in combination with a photosensitiser (a medicine activated by light) which can be used to kill parasites, cancer cells, fungal infection and even antibiotic resistant bacteria.
Most PDT methods use large hospital-based light sources, like lasers or arrays of inorganic light emitting diodes (LEDs), which are not available to treat patients at home and require lengthy stays in hospital.
The University of St Andrews have developed a wearable light source which can be used for PDT, meaning treatment can be taken to the patient in their own home, rather than being restricted to a few hospitals with specialised equipment. Light-emitting bandages, using organic light-emitting diodes (OLEDs) are also being developed to make thin, bright and flexible light sources for PDT.
OLED bandages allow treatment to occur outside the hospital setting and facilitate patients quickly returning to day to day activities. Wider applications for OLED bandages include treatment for many skin infections and conditions. The next step involves developing a solar charging system for the bandages, removing the need for batteries or an external electricity source.

The University of St Andrews are also developing and applying advances in optoelectronics in the field of biological assay to identify the effectiveness of drugs and investigating the possibility of other medical applications of organic light-emitting diodes.